 Waukeshahealthinsurance.com-
Waukeshahealthinsurance.com-
Ocala, Florida
Tampa Bay Times/KFF Health News
–
Fire Captain Jesse Blair drove his SUV through a mobile home park until he saw a small beige house with white trim and a radio.
There, Shaunice Slough waited on the stairs, wiping the sleep from her eyes.
“Good morning Shaunice,” Blair said. “How are you feeling today?”
“I've been good, I've been good,” he said. “much better.”
Three days earlier, Blair – a paramedic who leads the fire department's emergency medical team – met Sly at a nearby hospital. She overdosed on opioids. She took four bottles of overdose medication and dozens of chest compressions to get her breathing back.
At the hospital, Blair tells Slash about a free program that might help. He not only connects her to the rehab center, but also to her doctor's appointments and trips there. Best of all, she gets medication that eases the symptoms so she doesn't need medication to relieve the pain. Blair brings that medicine home every day.
“I have a son,” Blair, 31, said. I have to live for it.
Every morning since then, Blair has wanted to check in. He remembered the slaughter of appointments and helped with the clothes, food, bills.
And at the end of each visit, from a locker in the back of the car, he gave her two tiny, life-saving tablets.
Those tablets — a drug called buprenorphine — mark a major shift in the way counties in Florida and other states are addressing the opioid crisis. The idea: get addiction medicine to people who need it by connecting where they are. Sometimes, that's in the way. Sometimes, it's in the driveway of a big house with a swimming pool. Sometimes it's like a slaughter house on the steps.
*******
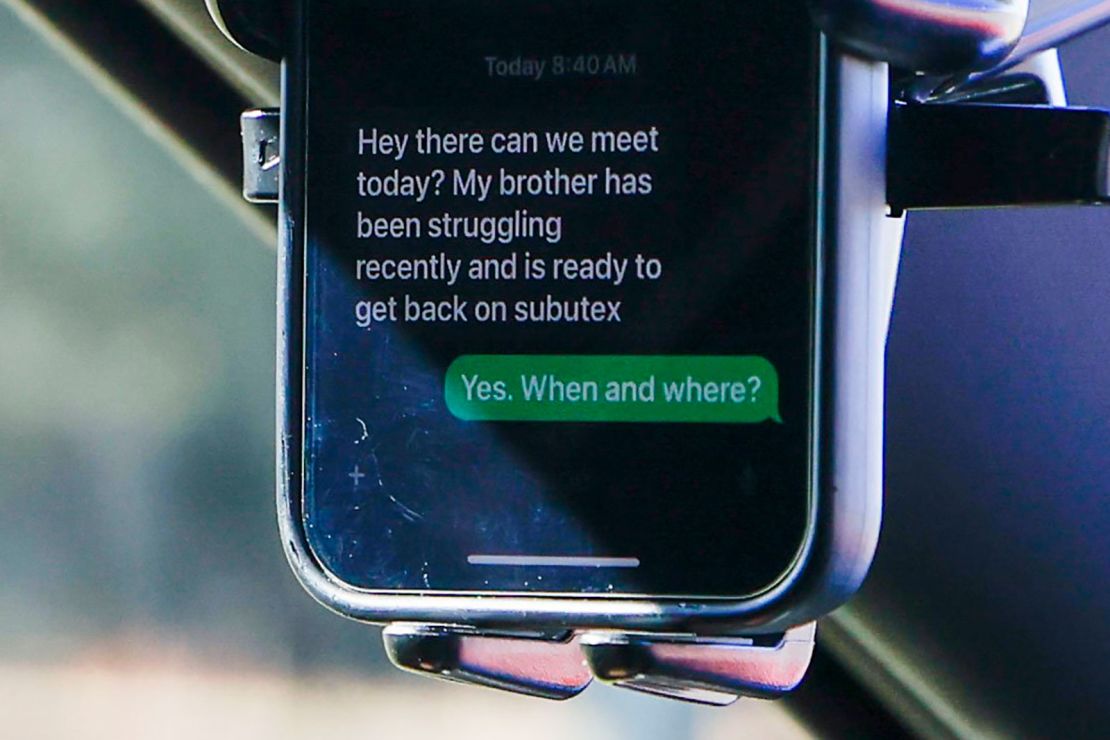
Not long ago, many people who could benefit from buprenorphine, commonly known by the brand name Subutex, could not get it.
Until recently, doctors needed a federal waiver to treat opioid use disorder. Amid misconceptions about treating opioid use disorder with medication, only about 5% of doctors nationwide have completed the training to become certified. And only in 2021 1 out of 5 people Those who may have benefited from opioid addiction medication were receiving buprenorphine or other drug treatment.

But as evidence grew to support the drug's effectiveness and the urgency to curb opioid deaths grew, Congress lifted the claim by the end of 2022, paving the way for greater access.
And in rare cases like Ocala, frontline medical professionals are starting to bring treatment to patients' front doors.
In Florida, the state-run Coordinated Opioid Recovery Network, known as the CORE Network, provides guidelines on drug distribution to areas affected by overdoses. Services provided through the network are free to patients, funded by the state's opioid settlement.
The network looks different in each of the 13 counties. Not all of them offer buprenorphine on hand. But the shared goal is to create a single entry point for services that are typically siled and difficult for patients to navigate, such as mental health care and residential support.
Easing the path for patients with convenient amenities and affordable price tags across the recovery landscape makes a meaningful difference.
“We know that the more people come into contact with services and are treated with respect, the more likely they are to reduce or stop using drugs,” he said. Susan ShermanProfessor of Public Health at Johns Hopkins University.
as a Opioid settlement dollars They keep coming, state officials say they hope to expand to more counties.
*******
Being a firefighter and paramedic satisfied Blair's need for adrenaline and his belief, informed in part by his Christian upbringing, that he was on this earth to help others.
In his 20s, he thought he would respond to car crashes and heart attacks, broken bones and punctured flesh. But after many years on the job at Ocala Fire Rescue, the calls began to change.
At first, Blair felt some displeasure at people taking too much. His team was suddenly responding to hundreds of such calls a year. He saw drugs as a moral failing. What if a grandmother has a heart attack or a child drowns while the team is on an overdose call?
Unlike other emergencies, he never felt like he could save a life when responding to an overdose. It was like delaying death.
Time and time again, a patient is pumped full of naloxone, an overdose reversal drug known by one brand name, Narcan, and admitted to the hospital. One Christmas, he responded to a man who overdosed five times in one shift.
“I do not understand. “I thought they wanted to die,” Blair, 47, said.
A decade earlier, the scope of the epidemic was already in full view on Blair's crew. The group seemed to be reacting to the excesses in the large houses in the affluent neighborhoods that were in the park and under the bridge.
One week, his group went to a house on a cul-de-sac with two kids and a swing set — the kind families take their kids trick-or-treating with.
His father had taken too much. Next week it was the mother.
“Money can cover any problem, but we've seen it from top to bottom,” Blair said.
Blair later came to understand addiction as a disease: a physiological change in a person's brain that traps them in a vicious cycle. Maybe it started with a post-surgery prescription pain reliever or an indulgence at a party, but he found out that most people weren't using drugs to get high. They used them to keep from getting sick.
“Imagine the worst cold you've ever had, then make it worse,” Blair says.
When someone addicted to opioids stops taking them, their body goes into withdrawal, often with tremors, nausea, fever, sweats and chills. Although people are rare He may die from opioid withdrawal syndrome. Still, historically, the emergency health care system has focused on reversing overdoses rather than treating the side effects that drive people back to drugs.
As Blair said earlier, I've seen patients discharged from the hospital with no more than a phone number for a recovery center. Getting an appointment can be challenging because of wait times or insurance issues, but because the patients aren't stable—they're isolating. To make it through the day, Blair said, they often reuse it.
“'Good luck, you're on your own,'” Blair said. “That's how it happened. And this does not work for a sick person.
Under Blair's leadership, Ocala Fire Rescue sought to end the revolving door by launching the Community Paramedic Program and the Ocala Recovery Project in 2020.
They modeled it after overdosing on fast-reacting groups that differ in makeup. Typically staffed by paramedics like Blair, these mobile teams connect people who have overdosed to services aimed at long-term stabilization. In some, a registered nurse accompanies paramedics in an ambulance or SUV. Others have a therapist or peer recovery coach on board. Some are bare-bones: a single responder with a phone 24 hours a day. Some contact patients through phone calls or home visits after overdoses are reported.
Others, like Blair's group, cut patients in the hospital.
Blair likens the system to a trauma alert — a message sent to medical centers to respond to fatal car crashes or shootings. When a trauma alert is issued, operating tables are cleared, CT scanners are set up, and responders are positioned to arrive.
“We've developed a similar system for binge drinking,” Blair said.
Now, when someone in Ocala overdoses on opioids, alcohol, meth or cocaine, an alert goes off that notifies Blair and his team, a peer recovery coach, a behavioral health specialist and a local recovery center.
His team usually drives an ambulance to the hospital.
The next day, team members follow up at the patient's home.
Then, last May, under the direction of the EMS medical director, Blair's team began providing addiction medicine to opioid users as well.
Since then, his team has connected 149 patients to treatment, Blair said. He said only 28 of them needed further intervention.
*******
Blair was skeptical when he first heard about buprenorphine.
How can giving more drugs help an addicted person?
That common response misunderstands the reality of addiction, he said Nora VolkowDirector of the National Institute on Drug Abuse.
People understand that one drug can be substituted for another, Volkow said. Instead, the use of medications such as buprenorphine is similar to those used to treat other psychiatric conditions such as mood disorders or depression.
Research shows that opioid addiction medication — including drugs like methadone — can help a lot Reduce the risk It increases overdose deaths, and keeping a person in treatment. But a Study outside New York University According to the Grossman School of Medicine, about 87% of people with opioid use disorder get nothing.
Such addiction medications work by stimulating opioid receptors in the brain.
Opioids — such as oxycodone or fentanyl — are what experts refer to as “total antagonists.” Think of an opioid receptor as a round plate. A whole character—like fentanyl—fits right in that bowl and holds the receptor tightly.
Buprenorphine is a “partial agonist”. It steps into the plate – and satisfies a need – but doesn't fully connect as a full character. Instead, it avoids withdrawal symptoms without getting high, so people don't get sick or crave illegal drugs. Second, it blocks the effects of other drugs, so a person can't overdose on other opioids like fentanyl or heroin while taking it.
And for someone who already uses opioids, an overdose from buprenorphine…
